Stem Cell Therapy Indications for Neurological Disorders in Phase II Clinical Trials
Stem cell therapies are being developed for several different indications. In April we reviewed stem Cell Therapy indications for cardiovascular disease that are in Phase II/III clinical trials. Cardiovascular disease indications are one of the largest concentrations of stem cell therapies in clinical trials.
Now, I have researched stem cell therapies that are in either Phase II or Phase III clinical trials for neurological disorders. For the purposes of this blog, I have only included information about ongoing trials or recently completed trials that are under review by the United States FDA (unless otherwise noted). I have not included trials that were stopped or were completed previously and have no future trials planned. While I have worked to include all current trials, please let me know if one is missing so that I may add it to the list.
Neurological disorders as an indication area includes therapies designated for Alzheimer’s disease, spinal cord injury, Parkinson’s disease, amyotrophic lateral sclerosis (ALS), and others. However there are only stem cell therapies for ALS and spinal cord injury in Phase II currently.
Amyotrophic lateral sclerosis (ALS)
Amyotrophic lateral sclerosis (ALS), is also known as Lou Gehrig’s disease and motor neuron disease. It is a type of neurodegenerative disease that affects motor neurons and causes degeneration and eventually death of the cells. Initially ALS causes muscle twitching and weakness, but over time as the motor neurons die, patients lose the ability to control muscles and muscle movement ceases. Unfortunately there is no cure for ALS and patients eventually die from the disease, as the ability to move, eat and breathe is lost.
Stem Cell Therapy Clinical Trials for ALS
Sponsor: BrainStorm Cell Therapeutics
Phase: Active Phase II Clinical Trial
Type: Autologous
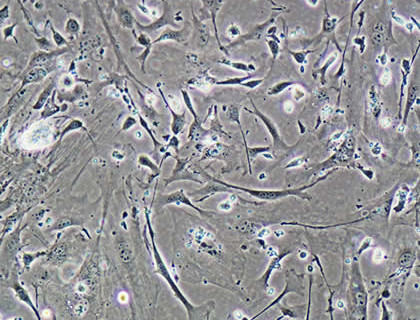
BrainStorm launched this study in June 2014. It is a multi-center study based in the United States and is designed to evaluate safety and efficacy of Brainstorm’s MSC-NTF or NurOwn product. The product is autologous mesenchymal stem cells secreting neurotrophic factors. The hope is that the stem cells will be able to deliver neurotrophic factors, which are important for neuron survival, directly to damaged areas. The product will be delivered via a single combined intramuscular and intrathecal administration of MSC-NTF cells in early-stage ALS patients. This product was designated orphan drug status by the FDA.
BrainStorm also launched a Phase II study in Israel in 2013. In this study, “trial participants received combined intramuscular and intrathecal administration of NurOwn cells in three cohorts with increasing doses. They were followed for six months after transplantation.”
BrainStorm also recently announced a technology collaboration with Octane Biotech, Inc. that resulted in a customized bioreactor for manufacture of BrainStorm’s NurOwn product. The press release states the “The proprietary bioreactor under development will provide BrainStorm with large-scale manufacturing capabilities, enabling it to achieve economies of scale for its autologous stem cell product.”
Sponsor: Neuralstem
Phase: Enrolling by Invitation Phase II
Type: Allogeneic
Neuralstem received FDA approval to begin its ALS Phase II trial in April 2013, after successful completion of its Phase I trial. The product NSI-566 is human spinal cord-derived neural stem cells. The Phase II study will look at safety and dose escalation and will be conducted at three centers in the United States. There will be five different dosing strategies evaluated. This product was also granted Orphan Drug status by FDA.
To deliver the cells, Neuralstem has developed a proprietary Spinal Cord Delivery Platform and Floating Cannula. To view a news report on the device being used during surgery during their Phase I study, please watch – http://www.myfoxatlanta.com/clip/7659207/
Spinal Cord Injury
Spinal cord injury is usually the result of a trauma to the spine that breaks or dislocates the bones of the spine and causes damage to the spinal cord. This kind of damage typically results in a decrease in body function and sensations below the point of injury. Some forms of injury allow for complete recovery and others will leave the patient permanently paralyzed. The clinical outcome largely depends on the severity of the injury and where the injury occurs along the spine.
Stem Cell Therapy Clinical Trials for Spinal Cord Injury
Sponsor: StemCells, Inc.
Phase: Ongoing Phase II
Type: Allogeneic
This study was initiated by StemCells in 2011 and is designed to evaluate safety and efficacy in patients with varying degrees of paralysis. The product HuCNS-SC, human neural stem cells, is delivered to patients who are 3 to 12 months post-injury via direct transplantation into the spinal cord. After receiving the transplant, patients will be given immunosuppression for nine months and will be evaluated regularly for 12 months with a separate long term four-year observational study beginning at the end of the trial. Efficacy clinical endpoints will include changes in sensation, motor and bowel/bladder function.